The knee: a key joint in our daily movements
The knee joint is one of the most complex and stressed joints in the human body.
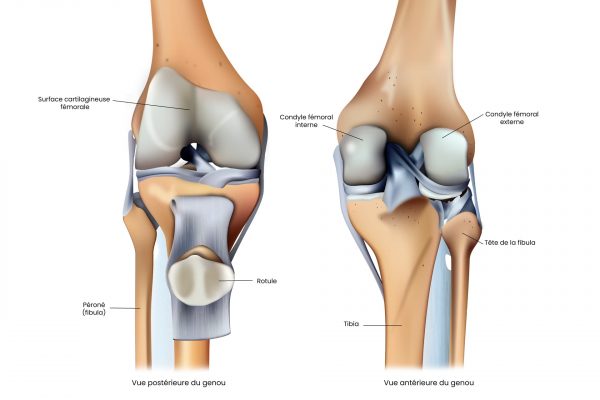
The bones that make up the knee
The femur
The femur is the longest and strongest bone in the human body. It extends from the hip to the knee, forming the upper part of the knee joint. The lower end of the femur has two condyles, the medial and lateral, separated by an intercondylar zone. The condyles are large, rounded protuberances that come into contact with the tibia to allow movement of the knee.
The patella
The patella is a small, triangular-shaped bone at the front of the knee. It is embedded in the tendon of the quadriceps femoris, the main muscle responsible for knee extension. The posterior surface of the patella is covered with cartilage and slides against the femoral trochlea, a groove located at the lower end of the femur. The patella plays an essential role in knee mechanics, acting as a lever to facilitate joint extension.
The tibia
The tibia is the longest and thickest bone in the leg, located on the inside of the leg, parallel to the fibula. The upper end of the tibia has two plates, the medial tibial plate and the lateral tibial plate, which are covered in cartilage and come into contact with the femoral condyles to form the femorotibial joint. Between the two plates lies the tibial spine, a bony structure that anchors the knee’s cruciate ligaments.
The fibula
The fibula is a long, thin bone located on the outside of the leg, parallel to the tibia. Although not directly involved in the knee joint, it is important for leg and ankle stability. The upper end of the fibula, called the fibular head, is connected to the tibia by ligaments, forming the proximal tibiofibular joint.
In conclusion, the knee joint is made up of three main bones: the femur, the patella and the tibia. Together, they provide a wide range of movement and stability for walking, running and other daily activities. Although not directly involved in the knee joint, the fibula contributes to the overall stability of the leg. Understanding these bone structures and how they interact is essential to understanding how the knee joint functions, and to identifying and treating any problems that may arise.
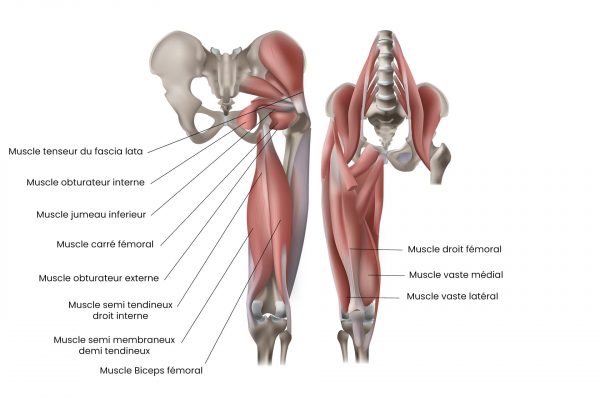
Muscles around the knee
The knee joint is a complex structure essential to the mobility and stability of the human body. The muscles that surround it play a vital role in knee function, enabling flexion, extension and rotation of the leg.
The main muscle groups of the knee :
The quadriceps femoris
The quadriceps femoris is a group of four muscles located at the front of the thigh. It comprises the vastus lateralis, vastus medialis, vastus intermedius and rectus femoris. These muscles converge to form the quadricipital tendon, which inserts onto the patella. The quadriceps femoris is responsible for knee extension, enabling the leg to be extended.
Hamstrings
The hamstrings are a group of three muscles located at the back of the thigh, comprising the biceps femoris (with its two chiefs: long and short), the semitendinosus and the semimembranosus. These muscles are mainly responsible for knee flexion, i.e. bending the leg. The biceps femoris is also involved in external rotation of the knee.
The muscles of the crow’s feet
The crow’s-feet muscles are a group of three muscles that insert onto the medial part of the tibia, forming a fan-shaped arrangement. They include the sartorius, gracilis and semitendinosus. These muscles help stabilize the knee and contribute to knee flexion and internal rotation of the leg.
The popliteus muscle
The popliteus muscle is a triangular muscle located at the back of the knee, extending from the femur to the tibia. It is responsible for internal rotation of the tibia during knee flexion, and helps stabilize the joint.
The gastrocnemius muscle
The gastrocnemius muscle is the most superficial muscle in the posterior part of the leg. It has two heads, the medial and lateral, which originate on the femur and join to form the Achilles tendon. Although primarily responsible for ankle plantar flexion, the gastrocnemius also contributes to knee flexion.
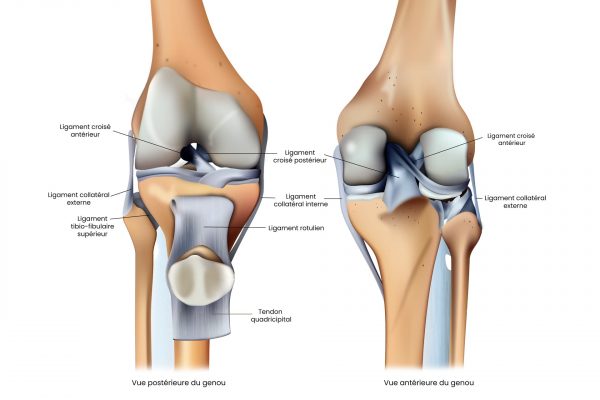
The ligaments that make up the knee joint
The ligaments surrounding the knee play a crucial role in maintaining stability and supporting the joint during movement.
The main knee ligaments :
The anterior cruciate ligament (ACL)
The ACL is a ligament located in the center of the knee joint, connecting the tibia to the femur. It is responsible for preventing excessive anterior translation of the tibia relative to the femur and stabilizing the knee during rotational movements. The ACL is one of the most frequently injured ligaments in the knee, particularly in athletes.
The posterior cruciate ligament (PCL)
The PCL is also located in the center of the knee joint, parallel to the ACL. It also connects the tibia to the femur, preventing excessive posterior translation of the tibia. The PCL is less frequently injured than the ACL, but is just as important for knee stability.
The tibial collateral ligament (TCL) or medial collateral ligament (MCL)
The LCT is a ligament located on the medial side of the knee, connecting the femur to the tibia. It is responsible for preventing excessive valgusization of the knee (outward movement) and stabilizing the joint during flexion and extension.
The collateral fibular ligament (CFL) or lateral collateral ligament (LCL)
The LCF is located on the lateral (outer) side of the knee, connecting the femur to the fibula. It prevents excessive varization of the knee (inward movement) and helps stabilize the joint.
The meniscofemoral ligaments
There are two meniscofemoral ligaments: the anterior meniscofemoral ligament and the posterior meniscofemoral ligament. These ligaments connect the menisci, which are cartilage discs between the tibia and femur, to the femur. They help stabilize the menisci and distribute forces during knee flexion and extension.
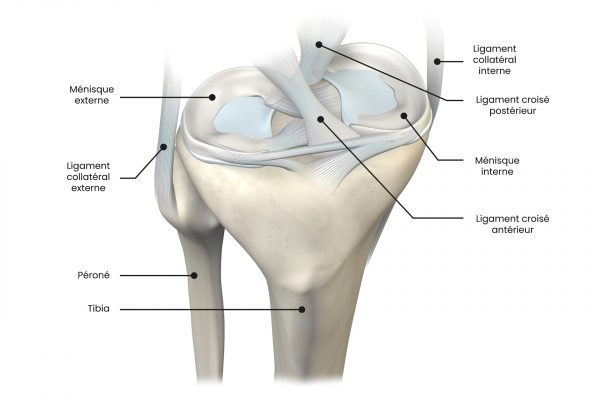
Knee menisci
Among the many structures that make up the knee, the menisci are essential for ensuring stability, mobility and load distribution within the joint.
Meniscus structure and function
- Meniscus composition
Menisci are crescent-shaped discs of cartilage located between the femur (thigh bone) and the tibia (leg bone). There are two menisci in every knee: the medial meniscus, on the inside of the knee, and the lateral meniscus, on the outside. These discs are composed mainly of fibrocartilage, a tough, elastic tissue.
- Main functions of menisci
The menisci perform several functions that are essential for the proper functioning of the knee:
- Load distribution: The menisci distribute the forces applied to the knee during walking, running or any other activity. They act as cushions to prevent the ends of the femur and tibia from rubbing directly against each other, thus reducing cartilage wear and minimizing the risk of osteoarthritis.
- Joint stabilization: menisci contribute to knee stability by ensuring an optimal fit between the femur and tibia during movement.
- Lubrication and nutrition: The menisci are involved in the distribution of synovial fluid, which lubricates and nourishes joint surfaces.
Nerves and vessels near the knee
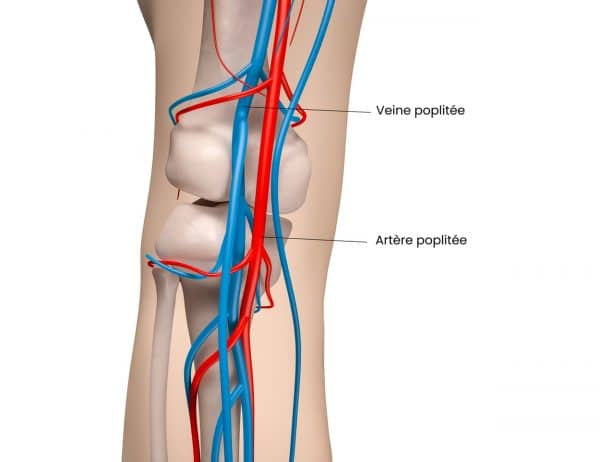
The arteries
Blood supply to the knee comes mainly from two sources: the popliteal artery and the geniculate arteries.
- Popliteal artery: The popliteal artery is a continuation of the femoral artery, which runs down the thigh and behind the knee (in the popliteal fossa), supplying most of the blood supply to the knee and leg. It then divides into the tibial and fibular arteries.
- Geniculate arteries: There are five geniculate arteries surrounding the knee, originating from the popliteal artery. They form a network of small vessels that supply blood to knee structures such as ligaments and menisci.
Veins
Oxygenated blood is returned to the heart by a network of veins located around the knee. The main knee veins are the popliteal, anterior and posterior tibial and fibular veins. They accompany the corresponding arteries and drain blood from the knee and leg structures.
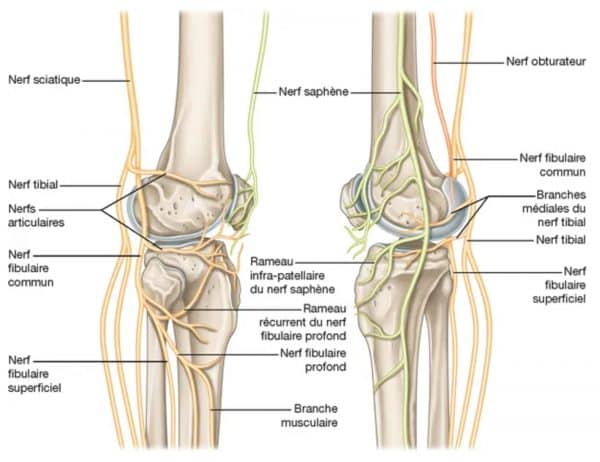
- Sciatic nerve: The sciatic nerve is the largest nerve in the human body. It crosses the buttock, runs down the back of the thigh and divides into two branches near the knee: the tibial nerve and the common fibular nerve. The sciatic nerve transmits nerve signals responsible for sensation and movement of the thigh, knee and leg muscles.
- Saphenous nerve: The saphenous nerve is a branch of the femoral nerve. It passes close to the knee joint and is responsible for sensation in the medial (inner) region of the leg.
- Common fibular nerve: The common fibular nerve is a branch of the sciatic nerve. It passes around the neck of the fibula and divides into superficial and deep fibular nerves. These nerves provide sensation and movement to the leg and foot muscles.
Evolution of the knee joint with age
The knee joint is one of the most stressed and complex joints in the human body. Over the years, the knee can undergo age-related changes, which can lead to reduced mobility and joint function.
- Cartilage wear: Cartilage is the soft, elastic tissue that covers the ends of the bones forming the knee joint. With age, cartilage can wear and thin, reducing its ability to absorb shock and allow smooth joint movement. This wear and tear of cartilage is often referred to as osteoarthritis of the knee.
- Reduced synovial fluid production: Synovial fluid is produced by the synovial membrane and helps lubricate the knee joint. With age, synovial fluid production can decline, leading to reduced lubrication and an increased risk of friction and cartilage wear.
- Reduced muscle strength: The muscles surrounding the knee, such as the quadriceps and hamstrings, are essential for supporting and stabilizing the joint. As we age, muscle strength and mass can diminish, leading to knee instability and an increased risk of injury.
Age-related pathologies
Hip pathologies can affect people at different stages of their lives. Here are some of the most common conditions, depending on the patient’s age:
In children and adolescents:
- Legg-Calvé-Perthes disease: this is a pathology that affects the femoral head, causing temporary interruption of the blood supply to this area, leading to necrosis and deformation of the bone. Symptoms typically include hip pain, lameness and reduced mobility. Children aged 4 to 8 are the most likely to be affected, and appropriate treatment can include physiotherapy, anti-inflammatories and even surgery in severe cases.
- Superior femoral epiphysiolysis: the femoral head moves in relation to the rest of the bone, causing instability and hip pain. It usually occurs during growth spurts and often requires surgical treatment to realign and stabilize the hip.
Adults:
- Trochanteric bursitis: inflammation of a bursa located on the greater trochanter, a bony prominence on the lateral side of the hip. This bursa acts as a cushion between the tendons and the bone to reduce friction during movement. Causes of trochanteric bursitis include trauma, overuse, muscle imbalances and structural abnormalities. Symptoms include lateral hip pain that worsens with movement or pressure. Treatment for trochanteric bursitis may include rest, ice, anti-inflammatories, physiotherapy and, in more severe cases, corticosteroid injections or surgery.
- Tendonitis: These are inflammations of the tendons that connect the thigh and hip muscles to the bone. They usually result from overwork or repetitive stress on the tendons, but can also be caused by trauma, muscular imbalances and anatomical anomalies. Symptoms of hip tendonitis include pain in the hip area, which may extend to the groin or thigh, as well as muscle stiffness and weakness. Pain may worsen with physical activity and diminish with rest. Hip tendonitis treatment aims to reduce inflammation and strengthen the surrounding muscles to prevent recurrence. Medical treatment approaches include rest initially, ice (debatable) and anti-inflammatories. Thereafter, strengthening and stretching exercises supervised by a physiotherapist should be resumed initially, and in more severe cases, corticosteroid injections or surgery.
- Osteonecrosis of the femoral head: Osteonecrosis (or avascular necrosis) is a condition resulting from loss of blood supply to part of the bone, leading to bone cell death and bone degradation. In the case of osteonecrosis of the femoral head, blood flow to the head of the femur is disrupted, leading to pain and possible damage to the hip joint. This pathology can occur following a fracture, hip dislocation, prolonged use of corticosteroids, or due to risk factors such as alcohol abuse or certain autoimmune diseases.
- Hip dislocation: Hip dislocation occurs when the head of the femur is forced out of the acetabulum. Dislocations can result from trauma, such as a car accident or fall, and are often accompanied by damage to surrounding ligaments, muscles and nerves. Hip dislocations require immediate medical intervention to restore the joint and minimize long-term complications.
- Inflammatory arthritis: Inflammatory arthritis, such as rheumatoid arthritis or ankylosing spondylitis, can also affect the hip joint. These autoimmune diseases cause chronic inflammation of the joints, leading to pain, swelling and reduced mobility. Treatment for inflammatory arthritis generally involves medication to reduce inflammation and slow disease progression, as well as exercise to maintain joint strength and flexibility.
- Iliotibial band syndrome (windshield wiper syndrome): Iliotibial band syndrome is a common condition among runners, cyclists and athletes. It is caused by inflammation and irritation of the iliotibial band, a thick connective tissue that extends from the pelvis to the shin. Pain usually occurs on the outer side of the hip or knee and can be relieved by muscle-strengthening exercises, stretching and training modifications.
- Piriformis syndrome: Piriformis syndrome is a condition in which the piriformis muscle, located in the gluteal region, causes pain and irritation of the sciatic nerve. This condition can cause pain and numbness in the buttocks, hip and sometimes down the leg. Treatment for piriformis syndrome generally includes stretching, muscle-strengthening exercises and, in some cases, anti-inflammatory drugs or corticosteroid injections.
In the elderly:
- Coxarthrosis: also known as osteoarthritis of the hip. This is a degeneration of the articular cartilage of the hip, leading to pain, stiffness and reduced mobility. The causes of coxarthrosis include aging, general wear and tear and genetic factors. Treatment for coxarthrosis may include anti-inflammatory medication, physiotherapy, lifestyle modification or, in more advanced cases, hip replacement surgery.
- Hip fractures: often due to falls and osteoporosis, a reduction in bone density that makes bones more fragile and prone to breakage. Hip fractures can lead to serious complications, including immobility, infection and a general decline in health. Prevention of hip fractures is based on reducing the risk of falls, improving balance and muscle strength, and managing osteoporosis. In the event of a hip fracture, medical management usually includes surgery, followed by rehabilitation to help regain strength and mobility.
Leave A Comment