The hip: the pivot of our mobility
The hip joint is a major joint in the human body, enabling great mobility and supporting our weight when walking, running and other activities.
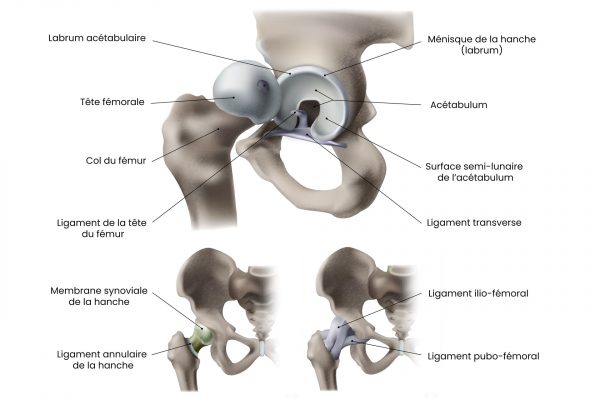
The bones that make up the hip
The hip is formed by the joint between two main bones: the hipbone and the femur. The iliac bone is part of the pelvis, while the femur is the longest and strongest bone in the human body.
Iliac bone
The iliac bone, also known as the coxal bone, is a broad, flat bone that forms the upper part of the pelvis. It’s made up of three parts: the iliacus, the ischium and the pubis. These three parts come together in adulthood to form a single structure, the iliac bone.
- The iliacus is the upper part of the bone and contributes to the formation of the iliac crest, a protruding structure that can be felt on the sides of the pelvis.
- The ischium is the lower, posterior part of the bone. It forms the ischium tuberosity, a bony protuberance on which we sit.
- The pubis is the lower, anterior part of the iliac bone. It joins the pubis on the other side of the pelvis to form the symphysis pubis, a cartilaginous joint.
The femur
The femur is the longest, strongest and largest bone in the human body. It extends from the hip to the knee and consists of several parts:
- The head of the femur is the rounded upper part of the bone that articulates with the hip bone to form the hip joint. It is covered with cartilage to facilitate movement.
- The neck of the femur is the narrow part that connects the head of the femur to the body of the bone.
- The greater and lesser trochanters are bony protuberances located at the junction of the neck and body of the femur. They serve as anchor points for several important muscles.
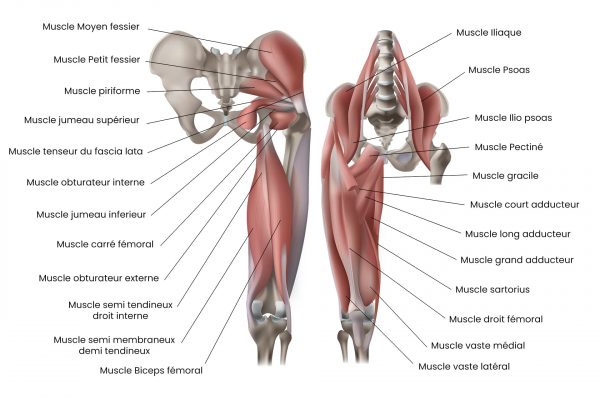
Muscles around the hip
- Gluteal muscles (large, medium and small): Responsible for hip extension, abduction and rotation.
- The psoas and iliacus (iliacus-psoas) muscles: Mainly responsible for hip flexion.
- Adductor longus, adductor brevis and adductor magnus muscles: Allow adduction of the hip.
- Quadriceps muscles: responsible for knee extension and hip flexion.
- Hamstring muscles (biceps femoris, semitendinosus and semimembranosus): Enable knee flexion and hip extension.
- The tensor fascia lata muscle: Contributes to hip flexion, abduction and internal rotation.
- The sartorius muscle: Allows flexion, abduction and external rotation of the hip.
- The piriformis muscle: Allows external rotation and abduction of the hip in flexion.
- The obturator internus and obturator externus muscles: They enable external rotation of the hip.
- Superior gemellus muscle: Also contributes to external rotation of the hip.
- The inferior gemellus muscle: This muscle helps with external rotation and adduction of the hip.
- The carré femoral muscle: Adduces and internally rotates the hip.
- The pectinate muscle: involved in hip adduction and flexion.
It’s important to keep these muscles strong and supple to preserve hip mobility and stability throughout life. Regular, appropriate exercise and stretching can help maintain hip joint health and prevent problems associated with age and wear.
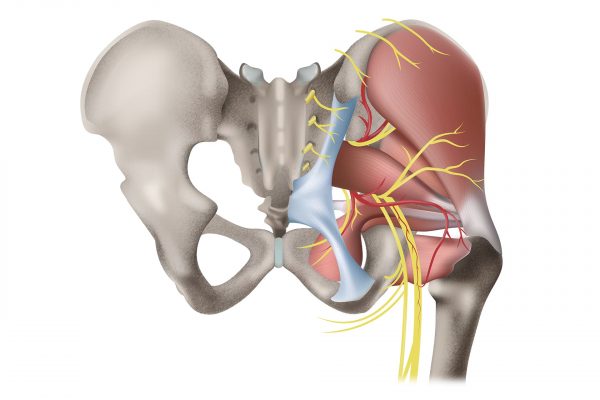
Nerves and Vessels nearby
The hip joint is richly innervated and vascularized.
The main nerves passing near the hip are :
- The femoral nerve: innervates the quadriceps muscles, enabling hip flexion and knee extension.
- The sciatic nerve: innervates the hamstring muscles, which allow flexion of the knee and extension of the hip, as well as other leg and foot muscles.
- The obturator nerve: innervates the adductor muscles and is involved in hip adduction.
Important blood vessels that pass near the hip include :
- Femoral artery: supplies most of the blood to the leg and hip.
- Circumflex iliac arteries: contribute to the vascularization of the femoral head.
Age-related changes in the hip joint
The hip joint undergoes a number of changes throughout life. In newborns and young children, the acetabulum is shallow and the ligaments are very flexible, allowing great mobility. As the child grows, the hip joint develops and strengthens. The acetabulum becomes deeper and the ligaments more robust, providing greater stability.
As we age, the hip joint can be affected by normal wear and tear, reduced bone density (osteoporosis) and loss of muscle strength. These changes can lead to reduced mobility and stability, as well as an increased risk of injury and pathology.
Age-related pathologies
Hip pathologies can affect people at different stages of their lives. Here are some of the most common conditions, depending on the patient’s age:
In children and adolescents:
- Legg-Calvé-Perthes disease: this is a pathology that affects the femoral head, causing temporary interruption of the blood supply to this area, leading to necrosis and deformation of the bone. Symptoms typically include hip pain, lameness and reduced mobility. Children aged 4 to 8 are the most likely to be affected, and appropriate treatment can include physiotherapy, anti-inflammatories and even surgery in severe cases.
- Superior femoral epiphysiolysis: the femoral head moves in relation to the rest of the bone, causing instability and hip pain. It usually occurs during growth spurts and often requires surgical treatment to realign and stabilize the hip.
Adults:
- Trochanteric bursitis: inflammation of a bursa located on the greater trochanter, a bony prominence on the lateral side of the hip. This bursa acts as a cushion between the tendons and the bone to reduce friction during movement. Causes of trochanteric bursitis include trauma, overuse, muscle imbalances and structural abnormalities. Symptoms include lateral hip pain that worsens with movement or pressure. Treatment for trochanteric bursitis may include rest, ice, anti-inflammatories, physiotherapy and, in more severe cases, corticosteroid injections or surgery.
- Tendonitis: These are inflammations of the tendons that connect the thigh and hip muscles to the bone. They usually result from overwork or repetitive stress on the tendons, but can also be caused by trauma, muscular imbalances and anatomical anomalies. Symptoms of hip tendonitis include pain in the hip area, which may extend to the groin or thigh, as well as muscle stiffness and weakness. Pain may worsen with physical activity and diminish with rest. Hip tendonitis treatment aims to reduce inflammation and strengthen the surrounding muscles to prevent recurrence. Medical treatment approaches include rest initially, ice (debatable) and anti-inflammatories. Thereafter, strengthening and stretching exercises supervised by a physiotherapist should be resumed initially, and in more severe cases, corticosteroid injections or surgery.
- Osteonecrosis of the femoral head: Osteonecrosis (or avascular necrosis) is a condition resulting from loss of blood supply to part of the bone, leading to bone cell death and bone degradation. In the case of osteonecrosis of the femoral head, blood flow to the head of the femur is disrupted, leading to pain and possible damage to the hip joint. This pathology can occur following a fracture, hip dislocation, prolonged use of corticosteroids, or due to risk factors such as alcohol abuse or certain autoimmune diseases.
- Hip dislocation: Hip dislocation occurs when the head of the femur is forced out of the acetabulum. Dislocations can result from trauma, such as a car accident or fall, and are often accompanied by damage to surrounding ligaments, muscles and nerves. Hip dislocations require immediate medical intervention to restore the joint and minimize long-term complications.
- Inflammatory arthritis: Inflammatory arthritis, such as rheumatoid arthritis or ankylosing spondylitis, can also affect the hip joint. These autoimmune diseases cause chronic inflammation of the joints, leading to pain, swelling and reduced mobility. Treatment for inflammatory arthritis generally involves medication to reduce inflammation and slow disease progression, as well as exercise to maintain joint strength and flexibility.
- Iliotibial band syndrome (windshield wiper syndrome): Iliotibial band syndrome is a common condition among runners, cyclists and athletes. It is caused by inflammation and irritation of the iliotibial band, a thick connective tissue that extends from the pelvis to the shin. Pain usually occurs on the outer side of the hip or knee and can be relieved by muscle-strengthening exercises, stretching and training modifications.
- Piriformis syndrome: Piriformis syndrome is a condition in which the piriformis muscle, located in the gluteal region, causes pain and irritation of the sciatic nerve. This condition can cause pain and numbness in the buttocks, hip and sometimes down the leg. Treatment for piriformis syndrome generally includes stretching, muscle-strengthening exercises and, in some cases, anti-inflammatory drugs or corticosteroid injections.
In the elderly:
- Coxarthrosis: also known as osteoarthritis of the hip. This is a degeneration of the articular cartilage of the hip, leading to pain, stiffness and reduced mobility. The causes of coxarthrosis include aging, general wear and tear and genetic factors. Treatment for coxarthrosis may include anti-inflammatory medication, physiotherapy, lifestyle modification or, in more advanced cases, hip replacement surgery.
- Hip fractures: often due to falls and osteoporosis, a reduction in bone density that makes bones more fragile and prone to breakage. Hip fractures can lead to serious complications, including immobility, infection and a general decline in health. Prevention of hip fractures is based on reducing the risk of falls, improving balance and muscle strength, and managing osteoporosis. In the event of a hip fracture, medical management usually includes surgery, followed by rehabilitation to help regain strength and mobility.
Leave A Comment